Chandigarh
14 July 2018
DIVYA AZAD
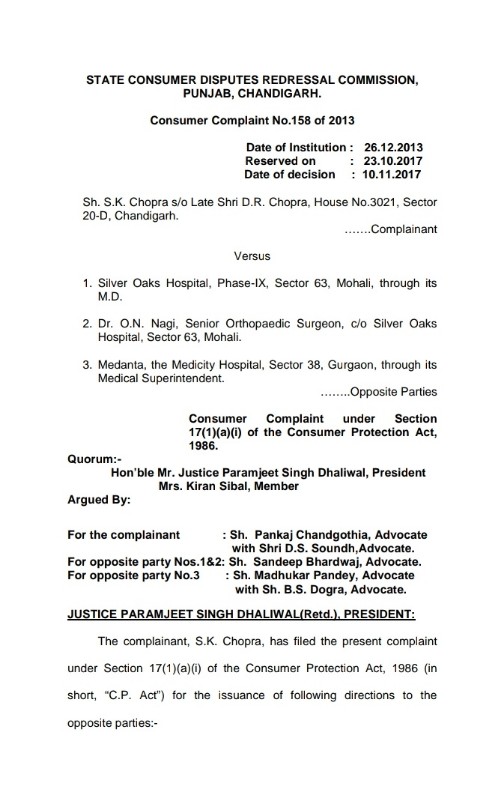
Justice(Retd) Paramjeet Singh Dhaliwal, President, Panjab State Consumer Commission, in a landmark judgment, has nailed celebrated Knee Surgeon Prof O.N. Nagi and Silver Oaks Hospital for committing negligence in performing Bilateral Total Knee Replacement ( “TKR”) on a 71 year old S.K. Chopra of Sector 20 Chandigarh.
Silver Oaks and Nagi are jointly and severally held liable to – i) Rs. 35,00,000/- in lump sum, as compensation, for the extra expenses and the sufferings he will have to bear in future including mental agony, harassment, avoidable pain, disability and suffering caused to the complainant along with interest at the rate of 7% per annum from the date of filing of the complaint i.e. 26.12.2013 till the date of actual realization; and ii) to pay Rs. 33,000/-, towards litigation costs. (TOTAL AMOUNTS TO 46,50,000/- as on date)(self calculation)
Earlier, SK Chopra of Sector 20 Chandigarh had filed a complaint through his advocate Pankaj Chandgothia, in the year 2013, that he was under treatment at Silver Oaks Hospital, Mohali (opposite party No.1) under the care of Dr. O.N. Nagi-opposite party No.2 for knee symptoms. He was advised Bilateral Total Knee Replacement (in short, “TKR”) surgery to improve the quality of life but it resulted otherwise. On 18.11.2010 pre-operative ECHO was carried out at Prime Diagnostic, which revealed Concentric left ventricular hypertrophy and Grade 1 diastolic LV dysfunction. On 18.12.2010 the patient was admitted for “elective” Bilateral Total Knee Replacement under the care of Dr. O.N. Nagi.
Pankaj Chandgothia, counsel for the complainant contended that the patient was posted for Bilateral TKR without disclosing or discussing his “high risk” status. The option for doing surgery of one knee at a time was neither discussed nor explained. Rather opposite party No.2 told that it was a routine surgery and would result in good quality of life. Even the pre-operative cardiac check/clearance was not done, which amounts to medical negligence.
Chandgothia argued that the patient was conscious and was in a position to discuss everything but high risk consent was not got signed from him after discussing the consequences and was kept in dark. The consent was got signed from his son under duress during surgery when the Doctors were struggling in the ICU/CCU to tackle the respiratory problem as a consequences of the heavy blood loss that had occurred during surgery. The son of the patient was informed that the patient was to be put on ventilator support and he must sign the documents. The patient’s son was made to sign various papers at that critical moment. During the surgery heavy loss of blood had occurred, which resulted into significant fall in hemoglobin necessitating blood transfusion and ultimately the patient was shifted to ICU.
As a result of the BTKR surgery, the patient developed severe respiratory distress, high BP and the chest examination of the patient revealed bilateral crept and he was treated on the lines of LVF and showed good response. On 30.12.2010 after about 9 days ECHO was done, which revealed LV diastolic dysfunction. On 31.12.2010 angiography was done then it transpired that it was a case of Coronary Artery Disease (CAD) Triple Vessel Disease. The patient had repeated episodes of chest discomfort and was advised Coronary Artery Bypass Graft (in short, “CABG”).
Chandgothia contended that all this was not explained either to the patient or to his relatives before carrying out surgery of both knees simultaneously, which as per the settled medical protocol and the medical literature, is not advisable in aged persons.
As a result, on 04.01.2011, at late night the patient had to be shifted in emergency state to Medanta Hospital.
Even after the TKR, the persistent pain did not subside.On 13.3.2011, elastic knee cap with patella retaining was advised. Again on 10.5.2011, Dr. Ashish Pal, an Associate of Dr. Nagi at Hospital noticed joint effusion and advised extension knee brace. Thereafter, the complainant also took second opinion at Fortis Hospital who advised knee aspiration and revision TKR for instability
On 13.11.2011 Dr. Nagi advised “release operation” for which he advised the patient to come to Sir Ganga Ram Hospital, Delhi and gave an estimate of Rs. 1 lakh. On 7.2.2013 Fortis Hospital, Mohali, has concluded that the right knee of the patient required a revision TKR and the estimated expenses were given as `3 lakh. The complainant had been visiting PGI for post-operative assessment and the complications. The Doctors of PGI have noticed various problems which included swelling and immobilized knee and have suggested for a repeat surgery. The patient/complainant visited various hospitals to find out the solution to the innumerable problems created by the surgery conducted by opposite party No.2. The opinion of the Government Medical College and Hospital, Chandigarh was also taken on 8.6.2013 and 14.10.2013, which revealed that the complainant was advised heavy medication and it was informed that apart from pain killers, the patient had to take various other medicines to tide over and bear the problems created by negligent treatment by the opposite parties.
Chandgothia contended that Bilateral Total Knee Replacement surgery by Dr. Nagi was against the standard practice which amounted to gross medical negligence.
Justice Dhaliwal while ruling on the necessity of Informed Consent has said that the consent is a legal requirement, not merely a procedural formality. It is most relevant in medical negligence case, specifically, when such case comes under judicial scrutiny. Except in medical emergency case, the informed consent must be taken before any investigation, procedure or treatment. In medical emergency, life-saving treatment can be given even in the absence of consent. Chapter 7 of Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002, Clause 7.16 of the Regulations reads as under: “7.16 Before performing any operation the physician should obtain in writing the consent from the husband or wife, parent or guardian in the case of minor, or the patient himself as the case may be. In an operation which may result in sterility the consent of both husband and wife is needed.”
In the area of medical negligence, the contentious aspects of medical care can be broadly categorised into three categories: A) Diagnosis: means medical condition/status of the patient; B) Advice: treatment options reasonable alternatives and risk attending on various options; and C) Treatment. The diagnosis and treatment are in the domain of doctor and the patient is a passive participant. When advice is being given to the patient, the patient assumes an active role. Then doctor’s function is to empower and enable the patient to make a decision by giving him relevant, sufficient and material information. The patient must make choices and decisions. The patient must be informed about the options for treatment, its consequences, risks and benefits. Why doctor thinks particular treatment necessary and appropriate for the patient. The prognosis and what may happen if treatment is delayed or not given. Failing to furnish correct sufficient information when obtaining consent may be a breach of duty of care. It amounts to negligence, failure to inform the patient. The patient must be given a reasonable amount of time to consider the information to make a decision. The allowing of cooling off period is for the purpose to give time to think over the decision or take advice so that patient does not feel pressurised or rushed to sign. On the day of surgery, the patient may be under strain, mental stress or under influence of the pre-procedure drugs which may hamper his decision-making ability. The doctor performing any procedure must obtain patient’s consent, no one else can consent on behalf of the competent adult. The consent should be properly documented and preferably witnessed as such consent is legally more acceptable. The video recording of the informed consent process may also be done with a prior consent of the patient for the same.
Before dealing with the merit of the case we would like to discuss with regard to the“Bolam Test”.There is a seismic shift in medical ethics and societal attitude towards the practice of medicine. Furthermore, the Medical Council had framed statutory regulations regarding the professional conduct, etiquette and ethics. This warrants legal tests to adjudicate the advice aspect of doctor patient relationship.The MCI Regulations as amended upto date clearly stipulate the need to respect the patient autonomy and doctor’s obligation to adequately inform the patient for self-determination. Nature of the patient doctor relationship has to be examined in the light of education and access to the knowledge of ordinary citizen. In the light of these facts and statutory provisions, the “Bolam Test”can no longer be applied to a doctor’s advice to his patient, unless it complies with the statutory provisions. The information given to the patient has to be examined from patient’s perspective.
The information disclosed is not limited to the risk related information. It should include: doctor’s diagnosis of the patient’s condition, the prognosis of that condition with and without medical treatment, the nature of the proposed medical treatment and the risks associated with it, the alternative to the proposed medical treatment, advantages and risks of the said treatment and the proposed treatment. The doctor must ensure that information given is “in terms and at a pace that allows the patient to assimilate it”, thereby enabling the patient to make informed decision.
In the present case, the Commission held that ” The patient was in a position to give consent himself and his case does not fall in any of the exceptions stated above. In view of the law laid down in the above noted authorities, we are of the view that the ‘Informed Consent’ of the patient was required to be taken by opposite party No.2, before conducting the surgery on the patient. However, they failed to produce on record cogent evidence that the consent document was got signed after making aware all the possible complications and that thereafter, the ‘Informed Consent’ of the patient or his son was taken at the relevant time, as a pre-operative procedure. The informed consent forms Ex.OP1/4 and Ex.OP1/6 have not been filled in by the doctor who explained the complications and risks involved. They are typed one and have blank spaces which have been in filled and signed by some person, may be a doctor. It has not come in evidence, who filled in the form, nor that person has been examined nor has his /her affidavit been placed on record. Even his/her name has not been disclosed in the entire proceedings. So, we hold that there is no cogent evidence that before getting the signatures of the patient or his sons, on the Informed Consent Forms, those were not read over and explained to the patient.
“To sum up in nutshell, the doctor/surgeon must take the consent of the patient before commencing a treatment/. No one can consent on behalf of a competent adult. The consent should be free and voluntary and be informed and based on intelligent understanding. The consent should be procedure specific. The consent obtained during the course of surgery is not a legally valid consent. When blood transfusion is anticipated, a specific written consent should be taken. The consent should be properly documented and witnessed. The surgical procedure consent is not sufficient to cover anaesthesia care. The fresh consent is necessary for a repeat surgery /procedure. All the above consents are subject to exceptions like emergency, medical emergency, therapeutic privileges and waiver situation. Simply going through the lists of risks and possible complications in the patient information sheet and consent addendum forms is not sufficient. The doctor(s) who discussed with the patient must document it. Preferably, video recording of the informed consent process and the procedure carried out must be done. Failing to comply all referred above amounts to negligence in medical care.”
“In view of the above discussion, we hold that in the present consumer complaint, ‘Informed Consent’ of the patient or his relatives/family members, was not taken by opposite party No 1&2 before undertaking the surgery on the patient. Hence, opposite parties Nos.1 and 2 are deficient in duty of care and resultant medical negligence.
HOSPITAL FAILED TO PRODUCE PROPER MEDICAL RECORD:ADVERSE INFERENCE
The bed head ticket and discharge slip have no documentation of the medical record. So, PGI Medical Board was not in position to opine about the negligence. So, we are of the opinion that the Medical Board opinion is not supported by any authentic proof and the same cannot be accepted as valid opinion. Hospital should have moved application before this Commission for permitting them to present the medical record before the medical board of PGI. But they failed to do so in spite of taking an objection that PGI Medical Board report is at their back and they were never associated with it. Once the material evidence, in the shape of medical record, is not forthcoming from the possession of opposite parties No.1 & 2 resulting into half-baked opinion, an adverse inference is to be drawn against OP No 1&2. Thus, they are guilty of suppressing the material facts from the PGI Medical Board and this Commission. In such circumstances, the said Medical Board’s opinion cannot be relied upon. Moreover, the medical record, which was produced before the Medical Board was not sufficient for it to opine about medical negligence. As such, the report of the Medical Board cannot be blindly accepted and both the parties cannot take the benefit of it. Otherwise also, the contention of the opposite parties that no expert was examined by the complainant to prove medical negligence on its part does not stand on its legs, as per the settled law. In “V. Kishan Rao Vs Nikhil Super Speciality Hospital & Another”, 2010(2) RCR (Civil)-929(SC),the Hon’ble Supreme Court held that the expert witness is not required to be examined in all cases of medical negligence. But while defining medical negligence, it was observed in para no.11 (Jacob Mathew’s case) as follows:- “11.The definition involves three constituents of negligence: (1) A legal duty to exercise due care on the part of the party complained of towards the party complaining the former’s conduct within the scope of the duty; (2) breach of the said duty; and (3) consequential damage.
In the opinion of this Court, before forming an opinion that expert evidence is necessary, the Fora under the Act must come to a conclusion that the case is complicated enough to require the opinion of an expert or that the facts of the case are such that it cannot be resolved by the Members of the Fora without the assistance of expert opinion. If a decision is taken that in all cases medical negligence has to be proved on the basis of expert evidence, in that event the efficacy of the remedy provided under this Act will be unnecessarily burdened and in many cases such remedy would be illusory.We do not think that in this case, expert evidence was necessary to prove medical negligence.
In a case where negligence is evident, the principle of res-ipsa-loquitur operates and the complainant does not have to prove anything as the thing (res) proves itself. In such a case, it is for the respondent to prove that he has taken care and done his duty to repel the charge of negligence.
The complainant has alleged medical negligence while performing Bilateral Total Knee Replacement surgery by OP No.2. The case of the complainant is that he was 70-year-old and hypertensive. The bilateral TKR in his case was not advisable as a result of which more blood was lost and consequent complications arose including cardiopulmonary problem. The orthopedic surgeons are split on their opinions of bilateral TKR. It suggests that age, physical health and mindset of the patient play a role in the final outcome. Recovery is more demanding for two knees than one. Looking at the literature and various articles on simultaneous versus staged bilateral arthroplasty specifically with reference to peri-operative risk comparison the rate of blood transfusion in bilateral TKR have been found to be greater than those in unilateral TKR. Cardiopulmonary and neurological complications are on higher side in bilateral TKR. Simultaneous bilateral TKR should be avoided in patient in a group of 70 years specifically when they have pre-existing comorbid factors. The post-operative reoperation rate is significantly higher in simultaneous bilateral TKR.
The doctors and the medical nursing staff of opposite party No 1&2 owed a duty of care to ensure that the complainant was provided with proper and skilled medical treatment including other health services and care in accordance with the generally accepted standards. In the present case, the patient’s preoperative ECHO was done on 18/11/2010 at Time Diagnostic Centre, which revealed concentric left ventricular hypertrophy and grade 1 diastolic LV dysfunction. The patient is 69-year-old. He was posted for surgery without discussing the high-risk status of the patient. Even the consent of the patient was not taken. It was obtained from the son when the doctors were struggling in ICU/CCU to tackle cardiopulmonary problem. The patient was put on a ventilator support. It was non-urgent/elective surgery.
The reply to the complaint has been filed by Dr. Akhil Bhargava and not by the surgeon nor he appended his affidavit on record as evidence. Even the material medical evidence has not been produced on record by OP No. 1 and 2. So adverse inferences are to be drawn against OP No. 1 and 2 as they have withheld the best evidence available with them. Therefore, the exact status of the condition of the patient has not been brought before this Commission.
It appears in the present case that opposite party No. 2 performed improper surgery to right knee. No record has been placed on record of this Commission with regard to documentation key steps taken in the procedure. Following the operation /surgery the condition of the patient became progressively worse. He experienced constant pain, swelling and difficulty in walking. This set in motion a series of consultation from other orthopedic surgeons and hospitals, diagnostic tests and possible treatment, culminating in the discovery by the other orthopaedic surgeons; Dr. Wadhwa, Dr. B. Raffle’s Hospital and PGI, Chandigarh that initial knee replacement was improper and require the debridement and revision TKR is to be done.This was diagnosed as a cause of crippling pain and associated problems. Had the right knee replacement been successful he would have had chances of living pain-free. Had the knee replacement been successful, on the balance of probability it would have lasted for 15 to 20 years before requiring revision surgery. The patient had been complaining to the surgeon about the knee swelling and numbness. Opposite parties Nos.1 and 2 have not placed on record radiology images to show that leg was adequately aligned during total knee replacement. The best evidence of skiagrams is not forthcoming from OP No.1&2.It clearly proves that treating surgeon and the hospital failed to treat the patient with the reasonable care and skill. Both opposite parties Nos.1 and 2 had breached their duty of care to the patient/complainant.
Thus, keeping in view the evidence on record, preponderance of probability and inferences, we hold that the complainant has been able to prove his case of medical negligence against opposite party No.1 and 2. It is true that medical negligence cases do sometimes involve questions of factual complexity and difficulty and may require the evaluation of technical and conflicting evidence. In the present case, complainant has been able to discharge the onus of proving on a balance of probabilities, the medical negligence averred against opposite party No.1&2 so far as bilateral TKR is concerned. We are of the view that certainly there was medical negligence on the part of opposite party No.1 & 2, specifically in intra-operative and postoperative care of the complainant/patient.
Quantum of Compensation: So far as the compensation is concerned, the complainant has claimed compensation under various heads. However, keeping in view the totality of the facts and circumstances of the present case, we are of the view that the patient/complainant deserves a compensation of `35,00,000/- in lump-sum for the extra expenses and the sufferings he will have to bear in future including mental agony, harassment, avoidable pain, disability and suffering caused to the complainant.
The following directions are issued to opposite parties Nos.1 and 2, who are jointly and severally held liable to pay the same:- i) to pay `35,00,000/- in lump sum, as compensation, for the extra expenses and the sufferings he will have to bear in future including mental agony, harassment, avoidable pain, disability and suffering caused to the complainant along with interest at the rate of 7% per annum from the date of filing of the complaint i.e. 26.12.2013 till the date of actual realization; and ii) to pay `33,000/-, towards litigation costs. 96. The compliance of this order shall be made by opposite parties Nos.1 and 2 within a period of two months from the date of receipt of certified copy thereof.